A compelling new study from researchers at Joslin Diabetes Center has shed more light on the mysterious connection between our diet, gut bacteria and mood. The study found that mice given a high-fat diet displayed greater depressive behaviors until microbiome-altering antibiotics returned their behavior back to normal.
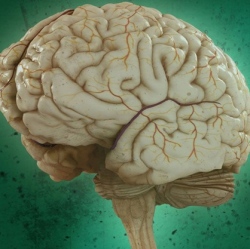
Microbiome research is undeniably one of the most exciting areas of medical research today. One of the most intriguing subsets in this field is the growing connections that link our gut bacteria and the brain. From PTSD to depression, researchers are finding interesting neurochemical effects stemming from the unique makeup of our gut microbiome.
It has long been known that people suffering from type 2 diabetes or obesity seem to be struck down with depression and anxiety at higher rates than the rest of the population. While this may seem like an obvious correlation, the psychological effects simply being a consequence of the disease, some researchers are beginning to suggest there may actually be more to it.
Several previous studies have found anxiety or stress-related behaviors in mice can be modulated through changes in the gut microbiome. This new work from the Joslin team set out to study how animals on high-fat diets can be behaviorally modified through microbiome alterations.
Earlier research from the same team established that mice fed a high-fat diet and bred to develop various metabolic diseases such as diabetes often had the onset of their diseases modulated by gut bacteria alterations. This new study set out to examine how a high-fat diet influences mood, and then how those mood changes can be subsequently disrupted through microbiome alterations.
The study initially showed that mice on a high-fat diet certainly displayed more clinical signs of depression and anxiety than those animals on a normal diet. But most interesting was the observation that when those mice on the high-fat diet were administered antibiotics they displayed behaviors that returned to normal.
The high-fat diet mice were administered two different broad antibiotics: vancomycin, to destroy gram positive gut bacteria, and metronidazole, which kills anaerobes. The antibiotics seemed to reverse any dietary induced negative behavior, but they also improved insulin-signaling in the brain, which was disrupted by the high-fat diet.
To confirm these changes were modulated through the microbiome, the researchers transferred gut bacteria from the experimental mice into a type of mouse engineered to have no gut bacteria of its own. In all cases the animals with the new, transplanted gut bacteria displayed behavior that mirrored the donor mice.
The research homed in on certain brain mechanisms that were being affected by these microbiome-alterations. It was discovered that many brain changes brought on by the high-fat diet were reversed when the antibiotics were administered.
"We demonstrated that, just like other tissues of the body, these areas of the brain become insulin resistant in mice on high-fat diets," says C. Ronald Kahn, senior author on the new study. "And this response to the high fat is partly, and in some cases almost completely, reversed by putting the animals [on] antibiotics. Again, the response is transferrable when you transfer the gut microbiome from mice on a high-fat diet to germ-free mice. So, the insulin resistance in the brain is mediated at least in part by factors coming from the microbiome."
At this stage, the researchers have not specifically targeted which bacteria could be causing the neurochemical changes, or what mechanism may be generating the effects. But it’s a compelling beginning and yet another piece of strong evidence suggesting the bacteria in our gut has a more profound effect on our well being than we ever previously realized.
Kahn also suggests that antibiotics, such as those used in the study, that alter a broad spectrum of gut bacteria would never be an end result for human treatments.
"Antibiotics are blunt tools that change many bacteria in very dramatic ways," says Kahn. "Going forward, we want to get a more sophisticated understanding about which bacteria contribute to insulin resistance in the brain and in other tissues. If we could modify those bacteria, either by putting in more beneficial bacteria or reducing the number of harmful bacteria, that might be a way to see improved behavior."
