Researchers claim they may be able to kill leukemic cells by blocking a small molecule called heme that acts as a kind of molecular “battery”. This could lead to the creation of new targeted drug therapies that block heme synthesis.
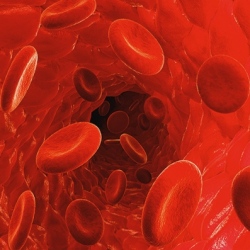
Heme is best known as a component of oxygen-carrying hemoglobin in red blood cells. However, heme also plays an essential role in transporting electrons in biological processes. Among these roles is the machinery for respiration in the cell.
While it has been suggested before that heme production affected leukemic cells, John Schuetz, part of St. Jude’s Department of Pharmaceutical Sciences, said: “Absolutely nothing was known about the role of heme biosynthesis before our work.”
Using the extensive St. Jude genomic database, the researchers searched for other genes that were abnormally switched on in a virulent form of AML.
The scientists pinpointed a particular gene called UROD as being highly activated in the leukemia – a critical finding since UROD is part of the molecular machinery that synthesizes heme.
“Our findings suggest two drug strategies to treat AML,” Schuetz said.
“One would be to target UROD, which would reduce heme biosynthesis. Such drugs would selectively affect leukemia cells, because they are so dependent on heme. The other strategy would be to use drugs to inhibit the relief-valve protein and at the same time administer a chemical that is a precursor of heme. This would cause a buildup of toxic molecules that are part of the heme synthesis pathway.”
AML is driven by a cancer-causing gene called MYCN. The study also revealed that MYCN-driven leukemias with the most over-activated UROD were far more lethal.
In the laboratory, the researchers found that cells with over-activated MYCN consumed more oxygen and depended on the production of heme to propagate – called self-renewal –as well as to become cancerous.
By suppressing heme production the researchers found that they were able to prevent self-renewal.
St. Jude researchers will now test whether drugs that suppress UROD function and heme-production machinery can effectively battle AML.
However, other cancers with an over-activated heme pathway might also be vulnerable to such a treatment strategy. Schuetz believes that one type of the brain cancer in particular – medulloblastoma – shows a similar over-activation of heme to AML.
