Many patients with advanced colon cancers who are successfully treated with immunotherapy and then stop those treatments appear to face little risk of tumor progression two years later.
That’s the main finding from a study that tracked outcomes for 64 people treated for metastatic colon cancer.
All were given approved immunotherapy meds such as Keytruda (pembrolizumab), Opdivo (nivolumab) or Yervoy (ipilimumab).
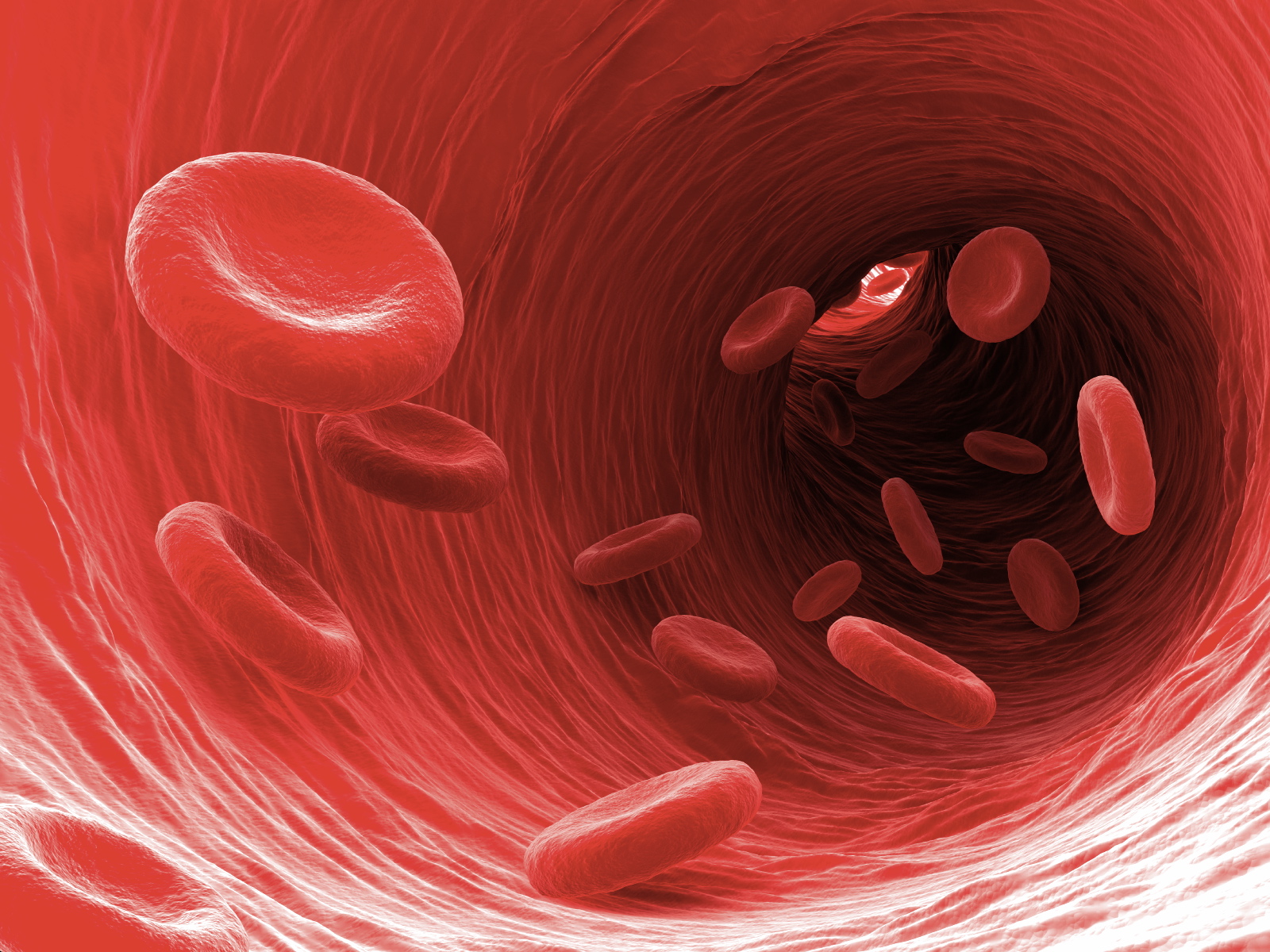
These drugs help activate the body’s immune system to target and destroy cancer cells.
The fact that most patients’ cancers did not progress after treatment discontinuation should help reassure patients who are offered that choice, said study senior author Dr. Van Morris.
“If you tell patients that, based on these data, there’s an 88% chance that their cancer won’t come back if they come off of therapy, I think they may be more accepting of that decision to stop treatment,” Morris said. He’s associate professor of gastrointestinal medical oncology at the University of Texas MD Anderson Cancer Center in Houston.
The advent of a class of cancer medicines known as immune checkpoint inhibitors (ICIs) has given many colon cancer patients new hope against the illness, even when it has spread (metastasized). Often, tumors will shrink or stabilize during ICI treatment, and at that point doctors may suggest discontinuing therapy.
Of course, “patients very understandably get afraid at the prospect of stopping a therapy which appears to be working and often does not cause many side effects,” Morris said in a news release from the American Academy for Cancer Research. “They’ve had a diagnosis of stage 4 colorectal cancer, and they wonder about the chance of their cancer coming back if they stop treatment. When we set out to do this study, we didn’t know the odds.”
In the study, 64 patients with metastatic colon cancer were treated with an ICI medication, either alone or in combination with a second immunotherapy drug. The patients experienced what doctors called a “durable benefit” from the treatment at the time that it was being given.
All 64 then stopped their immunotherapy regimen after receiving it for an average of about 18 months.
For 48 patients, treatment was halted because it had seemingly put the brakes on cancer progression. For another 16 patients, immunotherapy was discontinued due to drug side effects.
Tracked for almost two years after discontinuation, most (88%) patients showed no signs of cancer recurrence, Morris’ team found.
“The progression-free survival rate after cessation of immunotherapy was 98% at one year, 91% at two years, and 84% at three years post-treatment,” the researchers reported in the news release.
Outcomes were similar regardless of the reasons patients had decided to stop their immunotherapy.
For the minority of patients who did relapse after discontinuation, the only factor that seemed common was spread of cancer to the lungs, which Morris said needs further investigation.
The seven patients whose tumors did progress were placed back on an ICI regimen, and “all seven patients experienced a response or stable disease” when this was done, the researchers said.
Particular mutations in colon tumor cells didn’t seem to matter, Morris noted.
“We often hear from oncologists that they don’t feel comfortable stopping treatment on a patient with a BRAF mutation, for instance. But we did not see any association between mutation status and the likelihood for the cancer to recur,” he said.
The researchers stressed that the study was small, conducted at one cancer center and was retrospective, so larger, prospective studies may be required.
