If you put the wrong key into a lock, it won’t turn.
That’s because inside mechanical locks there are a set of pins that need to be in exactly the right position to allow a key to turn, and that position will be different for every lock. The ridges on the right key will be in the exact pattern needed to push the pins into the right place.
Use a key with a different pattern and the pins won’t line up properly.
Now, opening a lock with the right key is easy. But imagine you have 10,000 keys in front of you, and you’ve been tasked with finding out which one fits a specific lock. Not so simple, right?
That may not sound relevant to cancer research, but replace the word ‘key’ with ‘T cell’ and ‘lock’ with ‘cancer cell antigen’ and we’re back on track. And finding the right keys is the speciality of MATCHMAKERS.
MATCHMAKERS is an international team of researchers that was awarded up to £20m in funding from Cancer Research UK, the National Cancer Institute in the US and The Mark Foundation for Cancer Research through Cancer Grand Challenges earlier this year.
They’re developing computer models to decipher how T cells interact with cancer cells, or which keys fit which locks, to improve immunotherapies and match patients with the treatments best suited to them as individuals.
Search and destroy
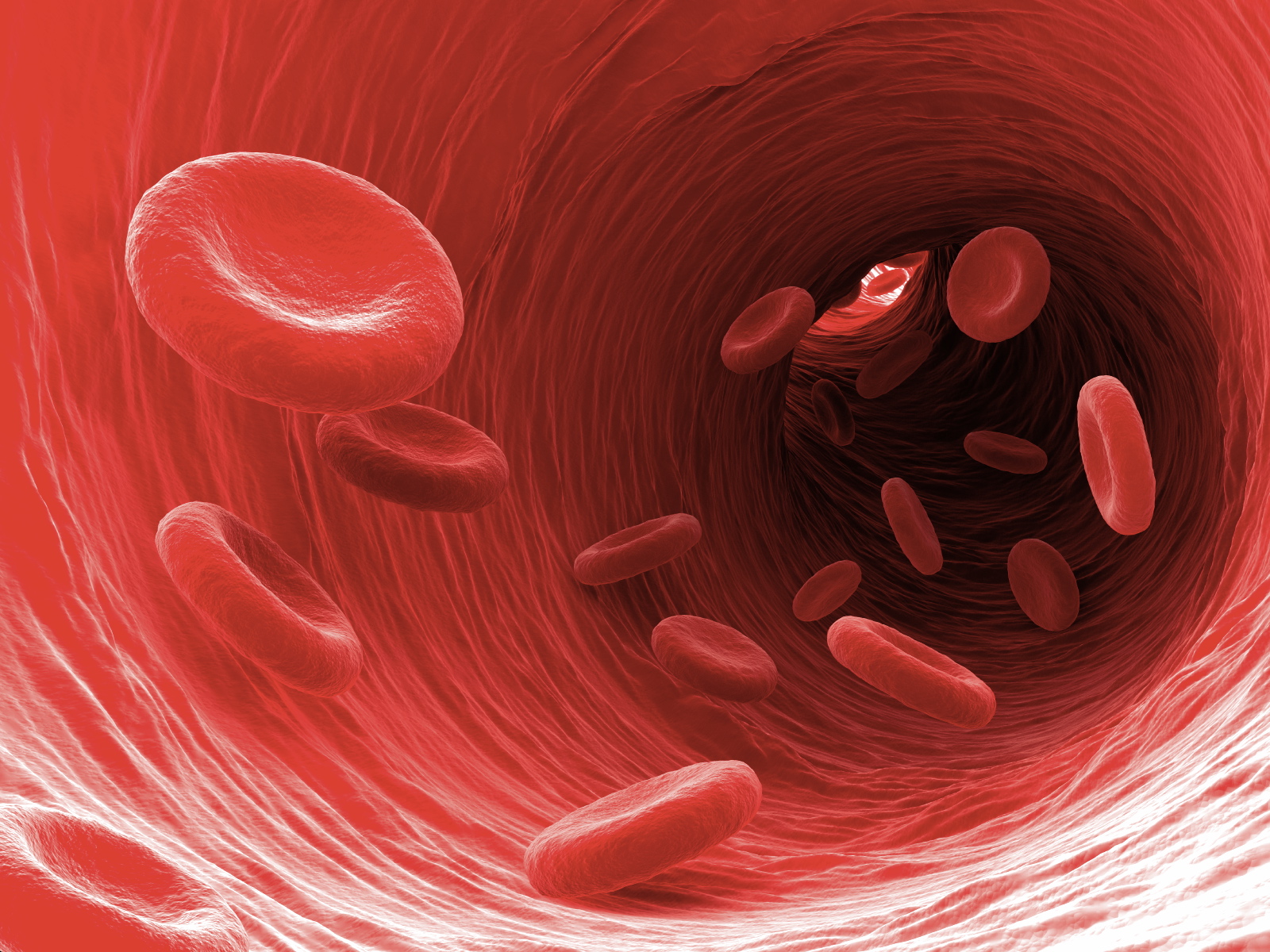
To rewind a little, T cells are a type of white blood cell that play an important role in our immune system.
Each T cell has an important protein called a T cell receptor on its surface. These are the keys in our analogy. In tandem, all the cells in our body – healthy cells, cells infected with viruses, bacteria we’ve picked up, and more – have molecules called antigens. These are the locks. If a cell could pose a threat to our health, it should have a tell-tale antigen that at least one of our T cells will recognise as alien.
When that happens – say if a cell has been infected by a virus – the T cell receptor will bind to the antigen on the infected cell and ‘mark’ it to be destroyed, either by the T cell itself or by other cells in our immune system.
The immune system is primed to respond to cancers in a similar way. Cancer cells can have different antigens to healthy cells, so T cells with the right receptors can bind to them and tell the immune system that they need to be destroyed.
Or at least, that’s how it’s supposed to work. But cancer cells are sneaky: they have their own mechanisms to prevent that from happening. As cancers grow, these cells can change in ways that help them to outsmart our immune system. Sometimes, they can ‘hide’ their antigens from T cells, or release chemicals that deactivate them. So, to give our immune system the best chance of destroying cancer cells, we need to stop cancer cells from escaping T cells.
That’s exactly what treatments called immunotherapies were developed for.
A heroic research effort
Immunotherapy is an umbrella term that covers treatments like monoclonal antibodies, checkpoint inhibitors, and cancer vaccines. Each treatment is slightly different, but all of them work by helping our immune system to recognise and attack cancer.
They help T cells to overcome the barriers that cancer cells try to put up, reactivating them as cancer-killing machines.
While a promising, and growing, type of treatment, immunotherapy doesn’t work for everyone, or on all types of cancer.
And currently, scientists aren’t entirely sure why.
It’s a hard problem to solve because all cancers are different. Even cancers of the same type may have different mutations in their cells, which means they’ll have different antigens. That makes it difficult for scientists to find out what antigens on the surface of cancer cells T cells are binding to, and how that differs in people that respond to immunotherapy versus people who don’t.
Think back to the problem I posed a minute ago. Scientists have thousands of keys in front of them, and they know that some of them fit the locks they want to open, but don’t know exactly what the locks look like.
So, to figure it all out, MATCHMAKERS are stepping in.
“We know that the T cells can recognise targets in the tumour, but we can’t always tell what they are,” says Dr Michael Birnbaum from the Massachusetts Institute of Technology, the team lead of MATCHMAKERS.
“And right now, our research lab could use cutting edge experimental methods to try to understand it for maybe one person’s cancer, but it really takes a heroic effort experimentally.
“We’re still very far from a good enough understanding to implement this in any way that would resemble a clinical test.”
Advancing us to the point where we could quickly and routinely test individuals’ cancers to see what treatments might be the most effective will also take a heroic effort. But that effort could help many more people. And MATCHMAKERS are up to it.
Across 12 labs in 10 different universities and hospitals across five countries, they’ve brought together clinicians, immunologists, engineers, and computer scientists to take on one of the biggest challenges in cancer research.
Target practice
Part of the reason revealing what T cells are seeing in someone’s cancer is so difficult is that it requires a lot of complex lab tests. These tests are time consuming and require currently unsustainable levels of investment and resource. Even with the most advanced technology we have available, they can take years.
MATCHMAKERS have a plan to overcome this issue.
“Advances in artificial intelligence (AI) mean that it should be possible to replace some of the lab tests with computer models,” says Birnbaum.
“These models would help us understand which therapies may work for a person, how effective they’re likely to be, and what the potential for side effects might be. So, it would really help match different people with the right treatments.”
The first step in building a model like that is what’s called ‘training’ the AI.
Think about AI models you might be familiar with, like ChatGPT.
ChatGPT can ‘understand’ and respond to questions and instructions because it was trained using a huge amount of information. From that information, it learned how words appear in context, and it uses that knowledge to predict what words are most likely to be used in response to specific requests, and in what order.
Now it’s been trained, you can give it new requests that it hasn’t seen before, and it can work out how to reply.
The AI developed by MATCHMAKERS would work in a similar way, but its job would be to predict what antigens each T cell receptor binds to. That is, if the team can train the model by showing it as many different types of T cell receptor and cancer cell antigen as they can.
Your own personal T cells
Up to this point, gathering that amount of data has been too difficult and time consuming to make a project like this possible.
But thanks to recent advances in technology, MATCHMAKERS are using techniques that can show us what receptors the T cells have, a process called sequencing, much faster. They’re also developing new techniques to improve the process even further.
They’ll be sequencing T cells taken from human and mouse tumour samples, as well as synthetically making T cells with different receptors in the lab to ensure the algorithm is trained on as many different examples as possible.
And if that weren’t enough, they’ll also be using techniques that show them the 3D structure of the receptors and the complexes they form when they bind to an antigen.
With all that information gathered, and subsequently used to train their AI algorithm, MATCHMAKERS are hoping to reach the point where they can show their model a T cell receptor and the model would predict the antigens it can recognise.
These predictions could then be used to design T cell receptors that are specific to an individual’s cancer.
The model could then be the basis for a simple test that can tell us exactly what keys open which locks – and open the doors to a whole new world of immunotherapies.
“If we understand what’s being recognised, we’ll also have the ability to design personalised vaccines,” Birnbaum says.
“We could say, ‘Here are the targets in your body and we should, therefore, formulate these vaccines in order to boost your own immune system against your tumour.’
“And, down the road, we see us having the ability to design new T cell receptors, potentially on a personalised basis.
“So, if we know that there’s a target in your tumour, but you don’t have T cells that are able to recognise it, we could design new receptors and reprogramme your T cells to create your own personalised cell therapy.”
