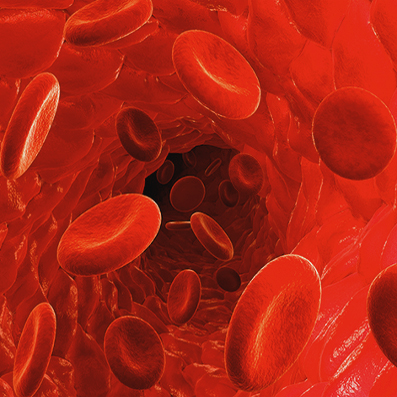
Passive antibody therapy is where the blood of patients who have just survived and are recovering from coronavirus is taken and given to the most at-risk people (old but healthy enough to take the treatment).
Can they also use the blood of people with mild cases? If we can do the proper tracing can we find mild cases, medium cases and use their blood too?
This means the 80% mild cases and the 7% more serious but not needing ICU cases could help provide immunity to seniors.
If we have 10,000 cases then maybe 8000-9000 could be mild but useful for immunizing the elderly (80+) in the hot zone. It also is used to improve the condition of those who are sick and need an immune system boost. We would be scrambling but we would be better at staying ahead of it and preventing deaths and ICU cases.
John Hopkins University is funding efforts to begin setting up antibody therapy operations for COVID–19 in the Baltimore area in the coming weeks. Doctors in New York are also investigating the treatment, Casadevall says, while internationally, Japan’s largest pharmaceutical company is looking at developing an antibody-based drug to combat coronavirus.
There are still a lot of unknowns, including how much convalescent serum is needed to be effective to protect people. China is already using this therapy on a few hundred people. They are providing the antibody boost to people and it has helped those sick with coronavirus to be less sick.
The blood of the strong survivors can be used to help those who are more vulnerable to coronavirus.
Historical and current anecdotal data on use of convalescent serum suggest it is safe in coronavirus infection, the high mortality of COVID-19, particularly in elderly and vulnerable persons, suggests that the benefits of its use in those at high risk for or with early disease outweigh the risks. However, for all cases where convalescent serum administration is considered, a risk-benefit assessment must be conducted to assess individual variables.
To deploy convalescent serum administration for COVID-19 the following six conditions must be met:
(i) availability of a population of donors who have recovered from the disease and can donate convalescent serum;
(ii) blood banking facilities to process the serum donations;
(iii) availability of assays, including serological assays, to detect SARS-CoV-2 in serum and virological assays to measure viral neutralization;
(iv) virology laboratory support to perform these assays;
(v) prophylaxis and therapeutic protocols, which should ideally include randomized clinical trials to assess the efficacy of any intervention and measure immune responses; and
vi) regulatory compliance, including institutional review board approval, which may vary depending on location.
Ideally, the use of convalescent serum would involve multiple centers, follow randomized control protocols, and have a single center as a governing body. Each of these conditions should be available in developed areas affected by COVID-19. At least one pharmaceutical company, Takeda, is gearing up to generate antibody preparations against SARS2-CoV-2 from COVID-19 convalescent sera. Producing highly purified preparations containing a high titer of neutralizing antibodies against SARS2-CoV-2 is preferable to convalescent sera given that these are safer and have higher activity. Unfortunately, such preparations will not be available for many months, whereas locally produced convalescent sera could be available much sooner.
