Compelling new research led by scientists from the University of Pennsylvania has used a novel machine learning method to analyze hundreds of brain scans from patients with schizophrenia. The results reveal significant differences in gray matter volumes, distinguishing two distinct types of schizophrenia and busting the previously held notion that all schizophrenia patients brains are the same.
In 2013, the American Psychiatric Association (APA) eliminated a number of different diagnostic classifications for schizophrenia, and rolled them all into a single category. The APA at the time noted these different subtypes of schizophrenia had “limited diagnostic stability, low reliability, and poor validity.” These former subtypes were not based on any objective physiological biomarkers, but instead relied on observations of behavior and symptoms. A number of impressive research breakthroughs over the past few years have offered new insights into the origins of schizophrenia, from links with gut bacteria and vitamin D deficiencies, to novel diagnostic methods using hair samples and eye scans.
However, those diagnosed with the disease have generally been gathered under the same umbrella of ‘schizophrenia.’ This is despite the extraordinarily heterogeneous nature of the disease with notable variations in symptoms and treatment responses from patient to patient.
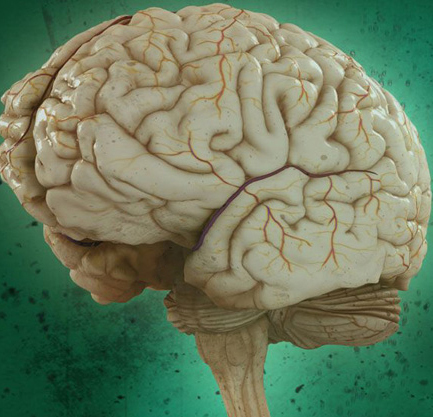
This new research set out to apply a machine learning method called HYDRA (Heterogeneity Through Discriminate Analysis) to over 300 MRI brain scans from schizophrenia patients spanning three continents. The results are challenging the prevailing notion that a general neuroanatomical feature of schizophrenia is lower volumes of gray matter in several brain regions.
“Numerous other studies have shown that people with schizophrenia have significantly smaller volumes of brain tissue than healthy controls,” explains Christos Davatzikos, principal investigator on the study. “However, for at least a third of patients we looked at, this was not the case at all — their brains were almost completely normal.”
Not only did nearly 40 percent of the schizophrenia patients display relatively normal gray matter volumes, but this large minority actually displayed small increases in gray matter in a middle brain region called the striatum, compared to the brain scans of a large healthy control group. A number of different variables, including medications and age, were accounted for, yet the researchers could not explain the prominent brain differences.
“The subtype 2 patients are very interesting, because they have similar demographic and clinical measures with subtype 1, and the only differences were their brain structures,” says lead author Ganesh Chand.
It is too early to tell exactly what distinguishes these two schizophrenia subtypes and the researchers are reluctant to hypothesize before further study is completed. But, this discovery will certainly offer new research pathways to better understand why some treatments may work better in particular patients. Daniel Wolf, co-senior author on the study, says this is the first step towards a future of personalized treatments in patients with schizophrenia.
“The treatments for schizophrenia work really well in a minority of people, pretty well in most people, and hardly at all in a minority of people,” Wolf explains. “We mostly can’t predict that outcome, so it becomes a matter of trial and error. Now that we are starting to understand the biology behind this disorder, then we will hopefully one day have more informed, personalized approaches to treatment.”
