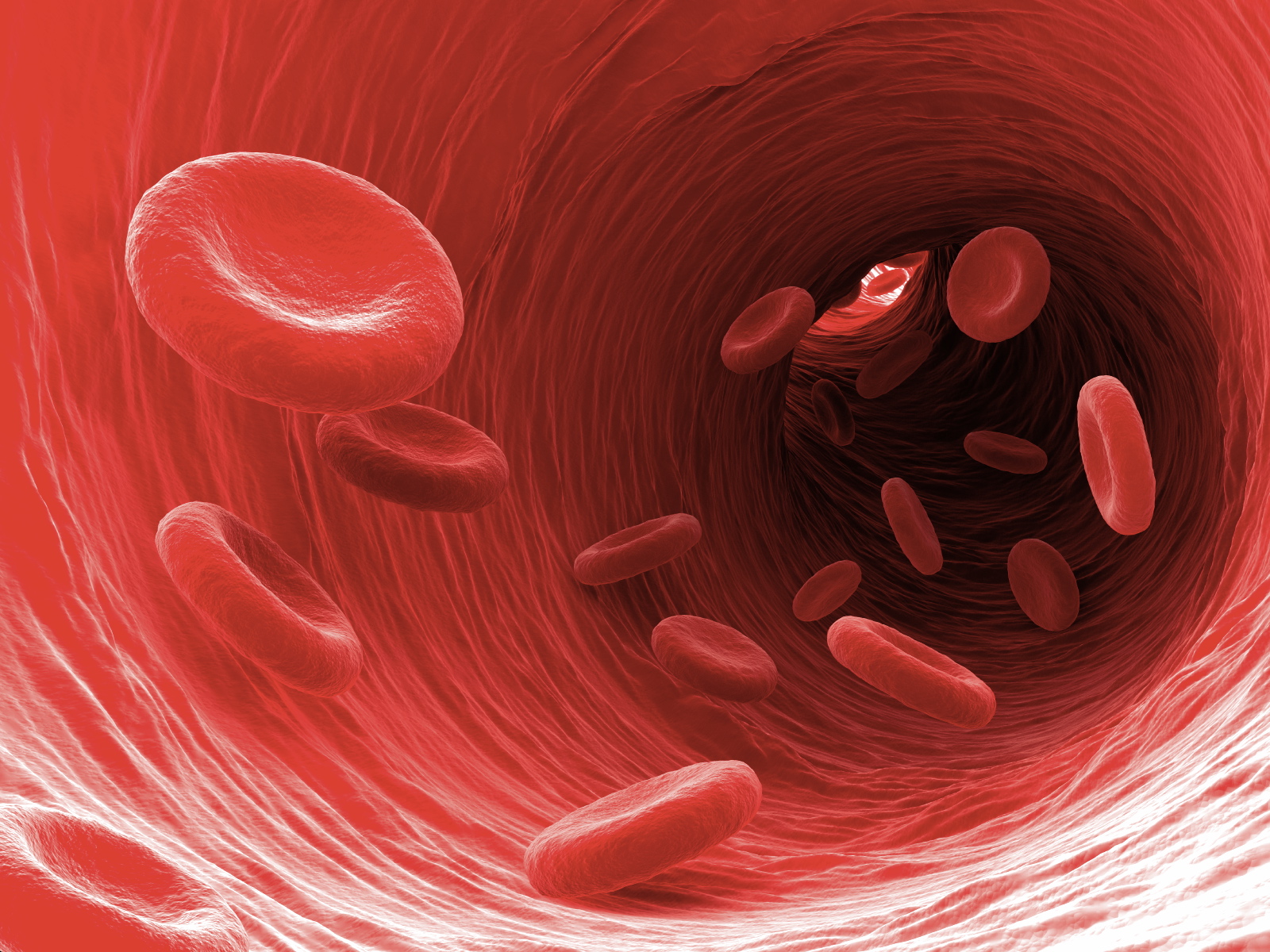
Even with a healthy diet and exercise, as our age slowly ticks up, so does the risk for clogged arteries, brittle blood vessels, and ultimately heart failure. Scientists have long sought to untangle the mystery of how aging links to increased risk of heart disease, a predominant killer of our time. It’s a tough problem: many biological aspects, spanning nature to nurture, can subtly influence heart health. With age, heart cells drastically change their function, eventually struggling to contract and release.
A new study published in Nature Aging looked deep into genetic code to unravel why this happens. Starting with a dozen volunteers spanning 0 to 82 years old, the team sequenced the entire genome of 56 heart muscle cells, or cardiomyocytes.
The result is the first landscape painting of genetic changes in the aging heart. As we age, the heart gets hit with a double whammy at the DNA level. Cells’ genetic code physically breaks down, while their ability to repair DNA erodes.
“As you age and get more mutations, you’re adding deleterious effects that might push the heart past a tipping point into disease,” said study author Dr. Ming Hui Chen, a cardiologist at Boston Children’s Hospital.
“It may get to a point where so much DNA is damaged that the heart can no longer beat well.” The results give us a birds-eye view of the aging heart.
Most heart failure cases happen in people older than 65, even when they’re relatively healthy-that is, without high blood cholesterol, blood pressure, or any other common risk factors.
“Some individuals at low or intermediate risk as based on traditional risk factors still experience heart disease, suggesting that additional, unidentified factors might be important,” the authors wrote.
What else is driving heart disease in the older population? Tackling the question, the team turned to a powerful genetic tool: single-cell sequencing, which transcribes the DNA chain of every analyzed cell.
“This is the first time somatic mutations have been looked at in the human heart at the single-cell level,” said study author Dr. Sangita Choudhury. The team honed in on how the heart cells’ DNA signature changes with age.
With age, these cells can accumulate genetic mutations. These mutations have previously been linked to coronary artery disease, a major cause of heart problems with age. Trying to capture mutational signatures leading to heart disease, the team took a deep dive into the genes of donated hearts from people spanning infancy to the elderly.
“Understanding the mutational signatures and their mechanism of formation might lead us to discover the mechanism of DNA damage and disease progression in the aging heart,” the authors said.
Looking further into the molecular underpinning of the signatures, the team found one potential culprit for heart aging and dysfunction: oxidative stress. Heart cells, for example, may end up with damaged DNA letters while simultaneously having their genome-repair mechanism destroyed.
“Because the heart is always pumping, it uses a lot of energy,” which produces chemicals that can damage DNA. What came as a shock was the heart’s special ability to ward off the damage.
Cardiomyocytes have the power to double up on their chromosomes, buffering against relentless assaults on their DNA. For now, the study only shows that somatic mutations increase with age, which correlates with damaged heart cells.
Whether DNA letter swaps cause heart injuries remains to be determined. The study is a first for dissecting heart disease at the single-cell level on a large scale. It’s like going from amateur binoculars to the James Webb Space Telescope-we can now analyze every single cell, like a star in the sky, by parsing its DNA inside an aging heart.
