Most people with cancer are diagnosed after they start experiencing symptoms, which are usually vague and hard to link to a specific cause. Typically, they’ll discuss those symptoms with their GP, who may only have a short appointment to work out what they might mean and decide on the best course of action.
That’s a tough job. GPs are crucial to the earlier diagnosis of cancer, but they have to deal with a lot of uncertainties.
The main problem is that the many potential signs and symptoms of cancer don’t usually point to cancer. Even when they do, it’s hard to tell which type of cancer might be causing them, so picking the right specialist referral route can be a challenge.
There aren’t currently many tools suited to helping GPs make these decisions. We’re looking at whether multi-cancer tests (MCTs) could change that.
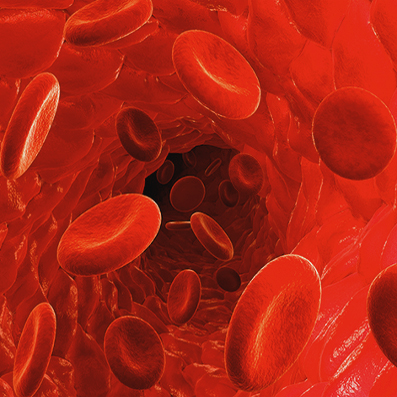
The emergence of MCTs represents an exciting opportunity to improve diagnosis and care for cancer patients across the pathway. Samples such as blood or urine could be tested for novel markers of many cancers to indicate if and where cancer is present.
In primary care specifically, MCTs could help GPs make informed decisions about which people with potential cancer symptoms should be referred for urgent cancer investigation.
As a result, MCTs could help GPs detect more cases of cancer earlier, which has the potential to improve outcomes and reduce cancer-related mortality. Equally, by making it easier to identify people who are unlikely to have cancer, MCTs could also help GPs find the true underlying cause of their symptoms more quickly – saving patients time and stress while reducing the burden on the NHS.
GPs are usually the first health professional people present to with symptoms. It’s up to them to rapidly assess whether or not a patient’s list of symptoms could indicate cancer, usually in a short appointment. They make their decisions based on both nationally agreed guidelines and their clinical judgement.
The guidelines GPs use set thresholds for urgent cancer referral using the probability that a person exhibiting a particular symptom or combination of symptoms actually has cancer. Some of these guidelines include abnormalities in routine blood tests, most of which are not specific for cancer but could indicate an increased risk of cancer when combined with signs and symptoms.
There are also a small number of triage tests used in primary care that support assessment of cancer risk. These tests help GPs identify which patients with signs and symptoms of cancer should be referred urgently for further investigation by a specialist and which ones they can safely monitor themselves. However, for many cancers, there is no triage test, or the available test is poor.
After a patient is referred, further investigations by specialists in secondary care either rule out cancer or lead to a cancer diagnosis.
The challenge for GPs is that signs and symptoms are generally poorly predictive for cancer
Some cancer signs and symptoms are specific (for example a breast lump indicating breast cancer). These are known as ‘red flag’ or ‘alarm symptoms’ and are associated with a higher risk of cancer. But evidence suggests that over 50% of patients subsequently diagnosed with cancer do not initially present to their GP with alarm symptoms. Instead, they present with non-specific symptoms (NSS).
Non-specific symptoms include weight loss, fatigue, abdominal symptoms like pain and bloating, nausea and vomiting, loss of appetite, and non-specific pain such as bone pain. Unlike alarm symptoms, which are usually closely associated with a specific type of cancer, these signs and symptoms could be caused by a range of different cancers or other non-cancer conditions. This presents a challenge as the guidelines often ask GPs to refer patients for investigations to see if they have cancer at a specific site.
People with NSS are more likely to have multiple visits to the GP and more primary care tests before referral, prolonging the time it takes to reach a diagnosis. While some GPs might still investigate or refer based on their clinical judgement or gut feeling, NSS often don’t meet the threshold for referral laid out in clinical guidelines. As such, people presenting with NSS are more likely to be diagnosed at a later stage or via emergency presentation at a hospital compared to those presenting with alarm symptoms.
New referral pathways have been created across the UK for patients with non-specific but concerning symptoms of cancer. These pathways recognise that NSS can be associated with many cancer sites, and that the risk someone with NSS has cancer is higher when you consider all those possible cancer sites together. This helps provide a more managed route for patients who do not experience alarm symptoms but are still at an increased risk for cancer. Although these pathways have helped establish a way of investigating cancer broadly across multiple sites, GPs must still make an informed decision for which patients with NSS require urgent investigation.
At the same time, only about 3% of people with red flag symptoms and less than 7% of people referred to NSS pathways have cancer. This is because the bar, or threshold, for referral in national guidance is relatively low (around a 5% probability of cancer).
The threshold is kept low to ensure that as many people as possible have their cancer diagnosed early, but it creates a capacity challenge. With diagnostic services under immense strain across the NHS, we need new tools to help GPs assess cancer risk and make more informed decisions about who to refer for urgent suspected cancer.
Multi-cancer tests could support GP decision-making. The additional information they provide could enable more accurate referrals for urgent cancer investigation and tell GPs which cancers to investigate for when a patient’s symptoms could be caused by many different types of cancer.
How could multi-cancer tests be used in primary care? In primary care specifically, MCTs could play an important role in reducing delays, first between a patient seeing their GP with symptoms and being referred for cancer investigation, and then between the referral and the eventual diagnosis. That means they could help the health service diagnose cancer earlier, which is associated with better outcomes, especially for people with fast-progressing cancers.
When we consider the sheer number of GP appointments per day where people could present with potential cancer symptoms, it’s easy to see how much value MCTs could bring. They could help under-pressure GPs triage patients and optimise referrals, improving patient experience and health system efficiencies.
For example, MCTs could help GPs:
Identify a higher risk of cancer – MCTs could give GPs confidence that they are referring the right people, even when they don’t have a red flag symptom to guide them.
Indicate which cancer pathway or investigation to refer them to – MCTs could be used alongside or instead of other diagnostic tests to help GPs identify the most appropriate cancer site to investigate. Alternatively, for NSS pathways, they could help to streamline follow-up diagnostic tests.
Identify those with a very low/no risk of cancer – A vast majority of patients who present at their GP do not have cancer. MCTs could help rule out cancer for these individuals, meaning they can be directed towards the most appropriate non-cancer investigations or work with the GP to continue to monitor their symptoms. This would improve patient experience by reducing invasive procedures and anxiety, as well as reducing strain on specialist services.
It’s not only primary care that could potentially benefit from MCTs. Specialists could also use MCTs to triage and prioritise urgent suspected cancer referrals they get from GPs.
