In 2001, a team of neurologists in San Diego began testing an experimental treatment for Alzheimer’s: Using tiny pieces of skin taken from the backs of eight patients with Alzheimer’s disease, the team isolated a long-living type of connective tissue cells.
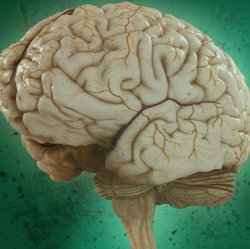
Then, using a virus as a delivery system, they genetically modified the cells to synthesize and secrete a potential therapeutic protein known as NGF, effectively turning the cells into little biological drug minipumps. Finally, the team implanted these mutant skin cells directly into each patient’s basal forebrain. Cells in this area are among the first to die from the disorder, and the scientists wanted to see whether NGF could help rescue the atrophy. Then they waited. For 10 years.
If this sounds crazy to you, you’re not alone. Fiddling with the human genome in a safe and effective way is notoriously difficult, especially when it comes to the brain. Yet against all odds, the gene therapy seemed to work. Published in the current issue of JAMA Neurology, the autopsy results show that the transplanted cells reliably pumped out NGF in the patients’ brains, which in turn enhanced the cells’ size and their ability to sprout new neural fibers.
What’s more, the treatment rescued vulnerable cells from dying, even if they already showed the trademark signs of Alzheimer’s pathology. In some patients, these beneficial effects lasted almost the entire 10 years after they first received the treatment.
The trial “very unequivocally (showed) that degenerating neurons can respond to NGF” lead author Dr. Mark Tuszynski told Singularity Hub.
