A compelling new study is claiming to have uncovered the missing link explaining how gum disease is associated with diabetes, cardiovascular disease and even Alzheimer’s.
Severe periodontitis, or gum disease, has long been observationally associated with broader systemic diseases.
Links between bad oral health and hypertension or even Alzheimer’s disease have frequently been detected but it has been challenging to determine whether the relationship is causal.
Now, in a robust study led by researchers from the University of Toronto, a potential mechanism has been found illustrating how oral disease may be exacerbating these other inflammatory conditions. The researchers set out to explore the activity of a type of immune cell known as neutrophils.
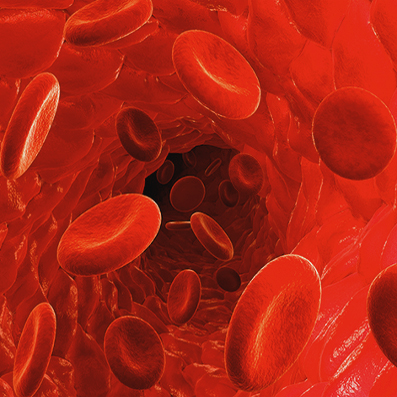
In the case of gum disease, neutrophils are a key part of the body’s natural immune response.
Initially using a mouse model of periodontitis, the researchers found an acute oral infection rapidly leads to heightened neutrophil production, and not just in the mouth. Elevated neutrophil counts were also seen in the animals’ bone marrow, suggesting the oral infection may be triggering broader systemic production of these immune cells.
After three weeks the researchers confirmed, through a variety of tests, enhanced systemic neutrophil activity.
Glogauer hypothesizes gum disease amplifying neutrophil activity may play a role increasing a person’s risk for severe COVID-19.
“There is evidence out there that patients with periodontal disease may be much more likely to have negative outcomes with COVID-19,” says Glogauer.
“Neutrophils are the cells that are at prime risk of causing cytokine storms. That’s the exact cell we show is primed with people with periodontal disease.”
