Pfizer and IBM researchers claim to have developed a machine learning technique that can predict Alzheimer’s disease years before symptoms develop. By analyzing small samples of language data obtained from clinical verbal tests, the team says their approach achieved 71% accuracy when tested against a group of cognitively healthy people.
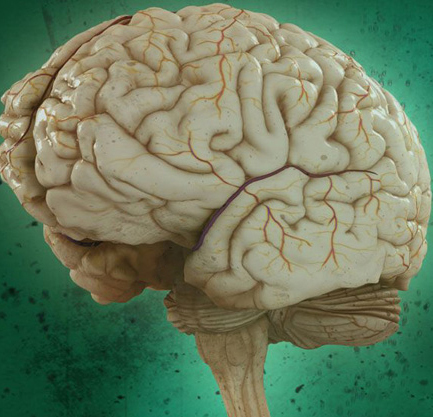
Alzheimer’s disease begins with vague, often misinterpreted signs of mild memory loss followed by a slow, progressively serious decline in cognitive ability and quality of life. According to the nonprofit Alzheimer’s Association, more than 5 million Americans of all ages have Alzheimer’s, and every state is expected to see at least a 14% rise in the prevalence of Alzheimer’s between 2017 and 2025. Due to the nature of Alzheimer’s disease and how it takes hold in the brain, it’s likely that the best way to delay its onset is through early intervention.
The disease is often detected too late to prevent it from accelerating.
IBM previously explored using AI to identify proteins that can predict the concentration of amyloid-beta, a peptide that changes before Alzheimer’s-related memory issues are apparent. And beyond IBM, others have investigated AI’s ability to spot the hallmarks of Alzheimer’s and dementia. For example, researchers at Unlearn.AI, a startup that designs software tools for clinical research, recently published a paper laying out a system that can anticipate the disease’s progression, projecting the symptoms that patients will experience. Another paper coauthored by researchers at the University of California, Berkeley, describes an AI system that can ostensibly predict Alzheimer’s disease from brain scans up to six years before clinical diagnosis.
But IBM and Pfizer claim this latest work differs “significantly” from previous research and the application of AI to aid in predicting Alzheimer’s. In contrast to studies predicting onset that focus on subjects showing signs of cognitive impairment, the researchers worked with samples that were collected before subjects in the study experienced the first signs of impairment. They also assessed the risk of Alzheimer’s in the general population instead of solely targeting high-risk groups, capturing a spectrum of people including those without a family history of the disease or other risk factors.
The study included 703 samples from 270 participants, half of whom developed Alzheimer’s symptoms before the age of 85. (The mean time to diagnosis of mild Alzheimer’s was about seven-and-a-half years.) From a language perspective, the researchers considered over 87 variables including misspellings, use of punctuation, uppercasing, verbosity, lexical richness, and repetitiveness. Beyond this, they looked at age, gender, education, visuospatial and executive reasoning, object naming, memory, attention, abstraction, and test results from the Montreal cognitive assessment MoCA.
The IBM and Pfizer team analyzed the transcriptions of participants’ samples with natural language processing, which allowed them to tap into AI to pick up subtleties and changes in discourse they might have otherwise missed. And after obtaining consent and approval from the Institutional Review Board of Boston University, they drew on data from original subjects (and their offspring and spouses) in the Framingham Heart Study, a population-based study overseen by the U.S. Public Health Service to investigate the epidemiology and risks for cardiovascular disease. In the Framingham study, enrolled people are assessed with the two-minute Mini-Mental State Examination speech test every four years and neuropsychological exams every year when possible cognitive decline is reported by a family member.
These steps resulted in a larger dataset than those used in other studies and made it possible to verify projections with real-life results. For example, if the model developed by the IBM and Pfizer coauthors predicted a 65-year-old Framingham subject would develop Alzheimer’s by age 85, they could check that person’s records to find out whether the subject had been diagnosed with the disease and when the diagnosis occurred.
Research has shown that much of the data used to train algorithms for diagnosing diseases may perpetuate inequalities. Recently, a team of U.K. scientists found that almost all eye disease datasets come from patients in North America, Europe, and China, meaning eye disease-diagnosing algorithms are less certain to work well for racial groups from underrepresented countries. In another study, Stanford University researchers claimed that most of the U.S. data for studies involving medical uses of AI come from California, New York, and Massachusetts.
Indeed, the researchers found evidence of bias within their own model, which predicted Alzheimer’s onset for participants without a college degree more accurately than for those with (76% versus 70%). It also attained higher accuracy with women compared with men (83% versus 64%), performing on average 2.61 times better for female subjects compared with males.
Cognizant of this, the IBM and Pfizer researchers say they plan to use datasets that expand on the geographic, socioeconomic, and racial diversity of subjects as their work continues. “This breadth of data is often very difficult to come by in terms of disease prediction, and access to it allowed us to train these models with precision,” they wrote in a blog post. “We [will] continue to train our algorithms while always respecting core principles of privacy, transparency, and consent.”
The team believes that if their work — which is published in The Lancet eClinicalMedicine — were to eventually reach production systems, it could help doctors determine the need for more complex and demanding psychiatric assessments, testing, and monitoring. It might also open up the door to more successful clinical trials, as those deemed at a high likelihood of developing the disease could enter trials for preventative therapies.
“Our vision is that one day clinicians will have multiple AI and machine learning tools to help identify if an individual is at risk of developing Alzheimer’s disease. [Our model’s accuracy] is a significant increase over predictions based on clinical scales (59%), which is a prediction based on other available biomedical data from a patient,” the team continued. “One day, doctors might be able to use speech and blood tests in conjunction with each other, leveraging AI to help them predict the risk of Alzheimer’s disease and laying the groundwork for preventative measures.”
