A new study evaluating the effectiveness of an eight-week program focusing on self-compassion and mindfulness found that it reduced symptoms of post-traumatic stress and improved quality of life and connectivity in parts of the brain that regulate emotions.
Many don’t meet the diagnostic criteria for full PTSD but experience post-traumatic stress symptoms, exhibiting clinically meaningful levels of functional difficulty and leaving them vulnerable to the development of future PTSD or other psychiatric diagnoses.
A new study by researchers at Murdoch University in Perth, Australia, has assessed whether an eight-week program centered around compassion and mindfulness is an effective way of treating people with PTSS. “Although post-traumatic stress symptoms can be debilitating, many people don’t seek treatment unless they experience a full post-traumatic stress disorder,” said Auretta Kummar, lead and corresponding author of the study.
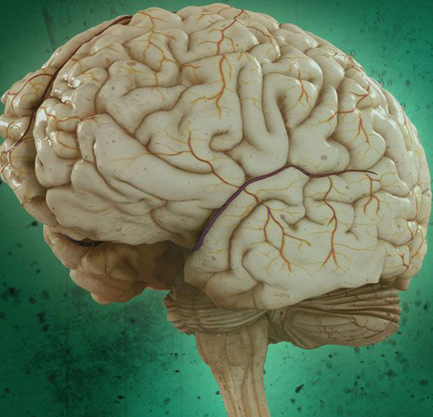
Recent studies have suggested that mindfulness supports emotion regulation – the ability to exert control over one’s own emotional state – during standard exposure treatments.
Evidence has emerged that self-compassion is a protective mechanism against PTSS. Mindfulness-Based Exposure Therapy is a 16-week non-trauma-focused intervention developed for combat-related PTSD. Integrating mindfulness strategies with exposure, the therapy was found to reduce symptom severity amongst veterans with clinical levels of PTSD. Using MBET as the basis, the researchers developed the CoMET program for civilians.
Participants were eligible if they had witnessed a traumatic event listed in the DSM-5 criteria for PTSD and exhibited at least one symptom from each PTSD symptom cluster but had not been diagnosed with the condition.
The study’s findings demonstrate that the CoMET program has potential as an intervention to alleviate PTSS by enhancing emotion regulation.
