Neuroscientists have identified key cells in the brain that control 24-hour circadian rhythms (sleep and wake cycles) as well as functions such as hormone production, metabolism, and blood pressure. This could lead to treatments for jet lag, neurological problems and metabolism issues.
The discovery may lead to future treatments for jet lag and other sleep disorders and even for neurological problems such as Alzheimer’s disease, as well as metabolism issues and psychiatric disorders such as depression.
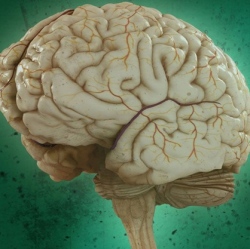
It’s been known since 2001 that circadian rhythms are generated within a specific area of the brain called the suprachiasmatic nucleus (SCN), a tiny region located in the hypothalamus.
But that region contains about 20,000 neurons that secrete more than 100 identified neurotransmitters, neuropeptides, cytokines, and growth factors, so researchers have not been able to pinpoint which neurons control circadian rhythms.
Now UT Southwestern neuroscientists report in the journal Neuron that they have found “a group of SCN neurons that express a neuropeptide called neuromedin S (NMS) is both necessary and sufficient for the control of circadian rhythms,” according to Dr. Joseph Takahashi*, Chairman of Neuroscience and Howard Hughes Medical Institute (HHMI) Investigator at UT Southwestern, who holds the Loyd B. Sands Distinguished Chair in Neuroscience.
NMS is a neuropeptide, a protein made of amino acids that neurons use to communicate. The researchers found in a mouse study that modulating the internal clock in just the NMS neurons altered the circadian period throughout the whole animal. The study also provided new insights into the mechanisms by which light synchronizes body clock rhythms.
“This study marks a significant advancement in our understanding of the body clock said senior author Dr. Masashi Yanagisawa, Adjunct Professor of Molecular Genetics, former HHMI Investigator at UT Southwestern, and current Director of the World Premier International Institute for Integrative Sleep Medicine at the University of Tsukuba in Japan.
The research was supported by the National Institute of Health and the Howard Hughes Medical Institute. So what’s causing these neuropeptide changes? Scientists have found that modern life, a cycle of inadequate exposure to natural light during the day and overexposure to artificial light at night, can mess with the body’s natural sleep pattern.
The solution may be to change our lighting, says University of Connecticut Health cancer epidemiologist Richard Stevens, who has been studying the effects of artificial lighting on human health for three decades. “It’s become clear that typical lighting is affecting our physiology,” Stevens says. “We’re learning that better lighting can reduce these physiological effects.
“By that we mean dimmer and longer wavelengths [yellow, orange, red] in the evening, and avoiding the bright blue of e-readers, tablets, and smart phones.” Stevens and co-author Yong Zhu from Yale University explain this in an open-access paper published in the British journal Philosophical Transactions of the Royal Society B.
The paper summarizes what we know up to now on the effect of lighting on our health, Stevens says. While short-term effects can be seen in [disrupted] sleep patterns, “there’s growing evidence that the long-term implications of this have ties to obesity, diabetes, depression, breast cancer, and possibly other cancers.”
The major culprit is electronic devices, which emit enough blue light when used in the evening to suppress the sleep-inducing hormone melatonin and disrupt the body’s circadian rhythm. (Blue light wakes us up in the morning, and reddish light, such as in a sunset, puts us to sleep.)
A recent study comparing people who used e-readers to those who read old-fashioned books in the evening showed a clear difference: those using e-readers showed delayed melatonin onset, Stevens said.
