Heart disease is the biggest killer in the Western world. A part of the problem is that even if one survives a heart attack, damage to the heart muscle results in the formation of thick scar tissue that can increase the chance of heart failure. Now researchers have found a way to improve the quality of the scar tissue in animal models, resulting in improved heart function following a heart attack.
The research centers on a protein therapy called recombinant human platelet-derived growth factor-AB (rhPDGF-AB), which had previously been shown to improve heart function in mice that had suffered a heart attack. In a new study aimed at bringing the treatment closer to human trials, a team set out to discover if it produced similar results in large animals, namely pigs.
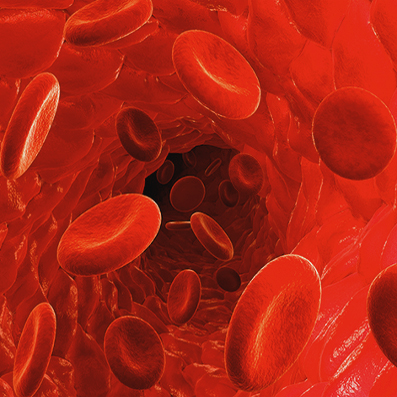
The researchers from the Westmead Institute for Medical Research (WIMR) and the University of Sydney found that when pigs that had suffered a heart attack received an infusion of rhPDGF, it did indeed prompt the formation of new blood vessels in the heart and led to a reduction of potentially fatal heart arrhythmia.
“This is an entirely new approach with no current treatments able to change scar in this way,” says Associate Professor James Chong who led the research. “By improving cardiac function and scar formation following heart attack, treatment with rhPDGF-AB led to an overall increase in survival rate in our study.”
Chong says that although the treatment didn’t affect the overall size of the scar, rhPDGF-AB improved heart function after the heart attack by triggering an increase in the alignment and strength of scar collagen fiber.
Current approaches focus on reducing scarring by restoring blood and oxygen supply to the heart as quickly as possible, but despite improving clinical outcomes, up to one quarter of patients who receive such treatment will still go on to develop heart failure within a year of suffering their first heart attack.
Additionally, there are many people who aren’t even aware they’ve had a heart attack or are unable to get to a hospital quickly, so a treatment that can be administered after the fact holds great potential.
“While we have treatment protocols in place, it’s clear that there is an urgent, unmet need for additional treatments to improve patient outcomes particularly after large heart attacks,” Chong says.
The team needs to conduct additional animal studies to establish safety and dosing, but hopes to start human trials “very soon.”
“This project has been developed over more than 10 years and we now have compelling data in two species for the effectiveness of this treatment,” says Chong, adding, “we now hope to further investigate the treatment, including whether it could be used in other organ systems impacted by scar tissue, such as the kidneys.”
