The cancer drug paclitaxel just got more effective. For the first time, researchers from the University of North Carolina at Chapel Hill have packaged it in containers derived from a patient’s own immune system, protecting the drug from being destroyed by the body’s own defenses and bringing the entire payload to the tumor.
“That means we can use 50 times less of the drug and still get the same results,” said Elena Batrakova, Ph.D., an associate professor in the UNC Eshelman School of Pharmacy. “That matters because we may eventually be able to treat patients with smaller and more accurate doses of powerful chemotherapy drugs resulting in more effective treatment with fewer and milder side effects.”
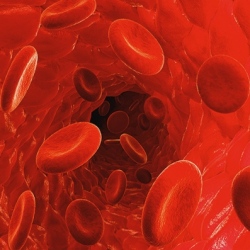
The work, led by Batrakova and her colleagues at the UNC Eshelman School of Pharmacy’s Center for Nanotechnology in Drug Delivery, is based on exosomes, which are tiny spheres harvested from the white blood cells that protect the body against infection.
The exosomes are made of the same material as cell membranes, and the patient’s body doesn’t recognize them as foreign, which has been one of the toughest issues to overcome in the past decade with using plastics-based nanoparticles as drug-delivery systems.
“Exosomes are engineered by nature to be the perfect delivery vehicles,” said Batrakova, who has also used this technique as a potential therapy for Parkinson’s disease. “By using exosomes from white blood cells, we wrap the medicine in an invisibility cloak that hides it from the immune system.
We don’t know exactly how they do it, but the exosomes swarm the cancer cells, completely bypassing any drug resistance they may have and delivering their payload.”
Paclitaxel is a potent drug used in the United States as a first- and second-line treatment for breast, lung and pancreatic cancers. It can have serious and unpleasant side effects, such as hair loss, muscle and joint pain and diarrhea, and it can put patients at greater risk of serious infection.
In their experiment, Batrakova’s team extracted exosomes from mouse white blood cells and loaded them with paclitaxel. They then tested the treatment, which they call exoPXT, against multiple-drug-resistant cancer cells in petri dishes. The team saw that they needed 50 times less exoPXT to achieve the same cancer-killing effect as formulations of the drug currently being used, such as Taxol.
“Accurately mapping the extent of tumors in the lungs is one of the biggest challenges in treating lung-cancer patients,” said Batrakova. “Our results show how powerful exosomes can be as both a therapeutic and a diagnostic.”
