For depression, magic mushrooms may indeed be magic.
Over the past decade, several of pioneering trials found that just one or two doses of psilocybin, the main component in magic mushrooms, rapidly pulls people out of severe depression.
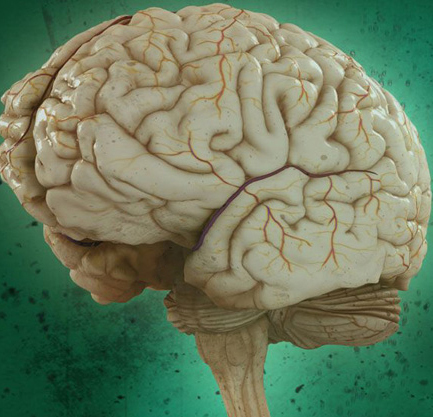
Combining brain imaging results from two trials of people with severe depression treated with psilocybin, the study found that the chemical shakes up global neural networks in the brain, essentially “Rebooting” how they communicate and forcing the brain out of its entrenched depressive funk.
“These findings are important because for the first time we find that psilocybin works differently from conventional antidepressants-making the brain more flexible and fluid, and less entrenched in the negative thinking patterns associated with depression,” said Nutt in a press release.
This rework of the brain’s connections might not be limited to depression. The brain is often locked in a state of negative cognitive bias, which draws people to think more negatively with a rigid idea about themselves and their future. This fundamental shift made some neuroscientists dig deeper: what’s going on with brain networks that supports those negative outlooks? As it happens, there are quite a few involved.
One is the default mode network, which covers wide-ranging connections of brain regions related to introspection and self-referential thinking and becomes overactive in depression. Unlike a healthy brain, one with depression is characterized by segregation, said Daws. In other words, depression makes the brain’s networks and information processing far more rigid.
Most antidepressants today zone in on a different aspect of depression-that is, lack of a brain chemical called serotonin-but don’t necessarily target these network-level changes.
Although psychedelics were broadly banned in the 1970s, they were previously examined in thousands of trials for their impact on the brain two decades prior. Tapping into modern technology, including functional MRI-a looking glass at how the brain reacts in real time-the studies hinted at psilocybin’s antidepressant potential.
In the new study, the team took advantage of brain scans from those two trials to uncover how magic mushrooms work in the depressed brain.
Peeking into their brains, the team analysed the brain scans with a method dubbed “Network modularity,” which looks at how connected or segregated different brain areas are. Comparing fMRI scans of peoples’ brains before and after psilocybin treatment, the team found increased connectivity just one day after psilocybin.
Previously segregated networks re-formed their social networks, causing an increase in brain connectivity, especially in networks normally disrupted by depression.
Using a metric called dynamic flexibility, the team also found that brain networks treated with psilocybin changed their community allegiance more rapidly over time.
Psilocybin doesn’t dampen brain activity-rather, it “Liberates the entrenched depressed brain, making it more integrated and flexible,” wrote the editors of Nature Medicine. The team especially highlights the need for replication-that is, to see if the same dynamic brain connectivity changes happen in separate groups of people.
The psilocybin trials took place in clinical settings with careful monitoring, and taking magic mushrooms in lieu of these guardrails to self-medicate for depression could be detrimental, if not outright dangerous.
While psychedelics haven’t yet fully proven themselves for therapy, the team is thankful for modern neuroscience technologies to start offering plausible models of their action on the brain.
