Hypertension (high blood pressure) remains the single most important modifiable risk for stroke, and the impact of hypertension and 9 other risk factors together account for 90% of all strokes, according to an analysis of nearly 27000 people from every continent in the world.
Although the same ten risk factors were important, and together accounted for 90% of stroke risk in all regions, the relative role of some individual risk factors varied by region, which the authors say should influence the development of strategies for reducing stroke risk.
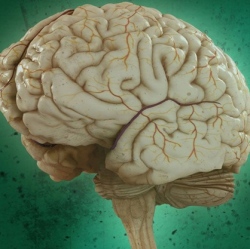
Stroke is a leading cause of death and disability, particularly in low-income and middle-income countries. The two major types of stroke include ischaemic stroke (caused by blood clots), which accounts for 85% of strokes, and haemorrhagic stroke (bleeding in the brain), which accounts for 15% of strokes. Prevention of stroke is a major public health priority, but needs to be based on a clear understanding of the key preventable causes of stroke.
To estimate the proportion of strokes caused by specific risk factors, the investigators calculated the population attributable risk for each factor (PAR; an estimate of the overall disease burden that could be reduced if an individual risk factor were eliminated [4]). The PAR was 47.9% for hypertension, 35.8% for physical inactivity, 23.2% for poor diet, 18.6% for obesity, 12.4% for smoking, 9.1% for cardiac (heart) causes, 3.9% for diabetes, 5.8% for alcohol intake, 5.8% for stress, and 26.8% for lipids (the study used apolipoproteins, which was found to be a better predictor of stroke than total cholesterol).
Many of these risk factors are known to also be associated with each other (e.g. obesity and diabetes), and when combined together, the total PAR for all ten risk factors was 90.7%, which was similar in all regions, age groups and in men and women.
Interestingly, the importance of some risk factors appeared to vary by region. For example, the PAR for hypertension ranged from 38.8% in western Europe, North America, and Australia to 59.6% in Southeast Asia, the PAR for alcohol intake was lowest in western Europe, North America, Australia and highest in Africa (10.4%) and south Asia (10.7%), while the PAR for physical inactivity was highest in China.
Atrial fibrillation (irregular heart rhythm) was significantly associated with ischaemic stroke (PAR ranging from 3.1% in south Asia to 17.1% in western Europe, North America, and Australia), as was a high apolipoprotein [ApoB]/A1 ratio (PAR ranging from 24.8% in western Europe, North America, and Australia to 67.6% in southeast Asia).
Prof Salim Yusuf says: "INTERSTROKE demonstrates that the majority of stroke is due to common modifiable risk factors. Our findings will inform the development of global population-level interventions to reduce stroke, and how such programmes may be tailored to individual regions, as we did observe some regional differences in the importance of some risk factors by region. This includes better health education, more affordable healthy food, avoidance of tobacco and more affordable medication for hypertension and dyslipidaemia."
"This is the first study that is adequately powered to explore stroke risk factors in all regions of the world and between stroke subtypes. The wider scope of this phase of our study lends a greater generalisability to the original INTERSTROKE results, and confirms the ten modifiable risk factors associated with 90% of stroke cases. The study also confirms that hypertension is the most important modifiable risk factor in all regions, and is therefore the key target in reducing the burden of stroke globally."
Three key messages can be drawn from this study.
1. stroke is a highly preventable disease globally, irrespective of age and sex.
2. the relative importance of modifiable risk factors and their PAR necessitates the development of regional or ethnic-specific primary prevention programmes, including priority settings such as focusing on risk factors contributing most to the risk of stroke in a particular region (as determined by PAR).
3. additional research on stroke risk factors is needed for countries and ethnic groups not included in INTERSTROKE, as well as definitive cost-effectiveness research on primary stroke prevention in key populations (eg, different age, sex, ethnicity, or region).
It should also be emphasised that stroke prevention programmes must be integrated with prevention of other major non-communicable diseases that share common risk factors with stroke to be cost-effective.
We have heard the calls for actions about primary prevention. Now is the time for governments, health organisations, and individuals to proactively reduce the global burden of stroke. Governments of all countries should develop and implement an emergency action plan for the primary prevention of stroke."
