All eyes were on big pharma company Biogen last week when it finally presented data from its two controversial Phase 3 trials into aducanumab, an Alzheimer’s drug that was originally labelled a failure early in 2019 before the results were reconsidered. Now, the company suggests aducanumab does indeed slow cognitive decline associated with Alzheimer’s and it’s looking to the US Food and Drug Administration (FDA) to approve the drug early in the new year.
The discontinuation of two large-scale final phase human trials into the efficacy of aducanumab early in 2019 sent shockwaves through the Alzheimer’s research community. The trials were halted after an early independent data analysis suggested the drug was not working and would not meet its primary endpoint.
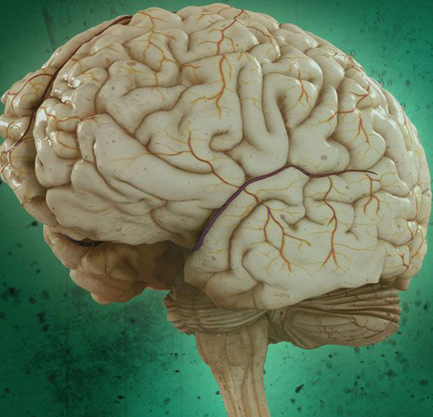
The failure of aducanumab came hot on the heels of several other prominent discontinued Alzheimer’s clinical trials, all focusing on reducing the accumulation of amyloid proteins in the brain.
The amyloid hypothesis argues the toxic aggregation of amyloid proteins into plaques in the brain is the primary pathological characteristic of Alzheimer’s disease. So, designing drugs that can either slow the aggregation of these plaques, or clear them entirely from a brain, has been the most promising path of research over the past couple of decades. Unfortunately, every single drug developed to target amyloid accumulations has failed in human trials, despite promising animal test results.
When aducanumab was classified a failure at the beginning of 2019, many experts suggested it could be the final death knell for the amyloid hypothesis. But in October a strange, and almost unprecedented, thing happened … Aducanumab came back from the dead.
Biogen suddenly announced the prior data analysis had been premature, and subsequent review had revealed the drug had indeed demonstrated statistically significant results in slowing the rate of cognitive decline associated with Alzheimer’s. Not only was Biogen resurrecting its interest in aducanumab, but it suggested the data was so strong that it was moving immediately toward filing for FDA approval.
The turnaround was so sharp it gave many in the Alzheimer’s research community whiplash. Biogen initially didn’t reveal specifics from the trial data to explain its dramatic change of direction. Instead, it simply claimed the early independent analysis of the trial data had only evaluated data gathered up to December 2018, despite the trials continuing until March 2019. Examining those extra months of data subsequently revealed patients receiving longer exposure to higher doses displayed significantly slower rates of cognitive and functional decline compared to the control group.
Last week Biogen finally revealed a more thorough indication of the trial data to researchers at the Clinical Trials on Alzheimer’s Disease conference in San Diego (CTAD). But not everyone was convinced by the presentation, despite Biogen’s enthusiastic rush to submit an FDA market approval application.
The CTAD presentation offered Biogen a platform to present its data from the two Phase 3 trials, and discuss why the research was resurrected. But Biogen’s big explanation hinged on explaining why only one of the two trials revealed positive results.
“EMERGE and ENGAGE were designed as twin studies, but due to some divergence in recruitment and changes in the protocol, different patients received different cumulative doses of Aducanumab,” explains Diego Gomez-Nicola, a researcher from the University of Southampton who has no affiliation with the Biogen research. “In EMERGE the patients received higher cumulative doses, and this led to significant improvement in the cognitive decline, results not observed in ENGAGE. These results are hugely important for the field, as for the first time demonstrate efficacy of a treatment for Alzheimer’s disease.”
So, in explaining why one trial failed and the other succeeded, Biogen suggests a protocol change during the trial resulted in a shift to the dosing strategy. Ultimately, more patients in the EMERGE cohort received higher doses of aducanumab for longer periods of time. It is this factor, among others, that led to the discordance between the two trials, according to Biogen. And on this basis, despite the confusingly mixed data, Biogen will proceed to market application with the FDA.
Not everyone in the Alzheimer’s research community is as positive about the aducanumab data as Gomez-Nicola. Critics of Biogen’s aducanumab research suggest all this data confirms is that the company needs to run a new Phase 3 trial to verify these muddy results. Derek Lowe, an independent researcher and chemist, calls Biogen’s push for FDA approval based on this data “irresponsible,” and says a new trial is the only reasonable way forward for the research.
“There was a protocol change during the studies that resulted in more patients getting the high dose, true – but after that change, sure, the high-dose patients managed to scrape over the line into statistical significance, but even the low-dose patients also showed better responses,” Lowe writes in a recent editorial discussing the newly presented aducanumab data. “Which makes no sense. That looks like an artifact to me; I don’t see any reason to assume that it isn’t, and I think that the burden is on Biogen to explain why it isn’t. The only way I can see making that case with a straight face is to run another trial with that hypothesis in mind from the start.”
Lowe is certainly not the only expert calling for a new trial to verify these results, but Biogen claims its move to market approval came from discussions with the FDA, implying the governmental body has, at least informally, suggested the current data could be enough to pass muster.
And now all eyes now turn to the FDA. Critics are already suggesting if the drug were to be approved on the basis of this data it would, “make mincemeat of the FDA’s approval standards.” Not only that, but as there are no other drugs on the market to treat early Alzheimer’s-related cognitive decline, the approval of this drug will set a number of precedents in terms of cost, efficacy and patient access.
