Researchers at Harvard University have come up with an alternative: A way to repair these holes using a minimally invasive catheter device, a pair of balloons, and UV light-activated glue. Their work was published today in Science Translational Medicine.
The new method is the first to combine the catheter and balloon technique with the light-activated glue, which was developed last year by the same researchers. The glue works via an adhesive-coated patch made of biodegradable materials, which attaches to the perforated area, whether it is in the heart, stomach, intestines, or another organ, and serves as a scaffold to allow the tissue to grow and heal. Once the tissue has completely healed, the patch melts away. Since this UV light-activated adhesion method was developed, the researchers had trouble finding a way to get the adhesive patch to the affected area without using invasive techniques.
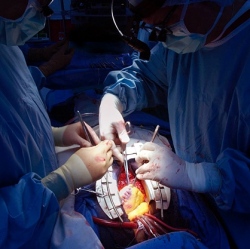
Their new technique uses a thin hollow plastic tube called a catheter to guide the patch to its destination. During the procedure, the catheter is first advanced to the organ (either through an endoscope to digestive organs or through a catheter to the heart or bladder) and then slowly guided through the perforation or defect. Once that’s secure, a system of two balloons helps put the patch in place
. First the balloon on the outside of the organ inflates, which deploys the adhesive patch onto the affected area. Then a balloon on the inside of the organ is inflated, which causes the ultraviolet light to turn on. This activates the adhesive properties of the glue and forces the patch to stick onto the tissue. Once finished, the balloons deflate and the catheter is removed. The patch sits on the hole until the tissue heals itself. Once it’s done, the patch dissolves.
The use of this new method in real patients is still far off, however, as the point of this early study was simply a proof of concept. The initial experiments did show some limitations, including the flexibility of the catheter device. In future studies, the researchers hope to use multiple fiber bundles and a cone-shaped tip to increase flexibility and access, which they hope will bring the device closer to being ready for clinical use.
